Cervical Cancer Screening Kit
EN | FR
Note:
-
If you already have a kit at home, please complete the kit and reply form as soon as possible, and mail.
-
If you received a letter from CervixCheck inviting you to request a cervical cancer screening kit, we are not able to fill anymore requests. To make an appointment for a Pap test contact your healthcare provider, or click here to find a Pap test clinic near you.
To learn more about HPV, HPV vaccination, and Pap tests, click here.
Prevent Cervical Cancer
Cervical cancer is caused by human papillomavirus (HPV). Over 80% of people who have ever had sexual contact will have at least one HPV infection in their lifetime. Most people show no signs or symptoms of the virus. HPV can cause abnormal cells to grow on the cervix which may or may not lead to cervical cancer. The best ways to prevent cervical cancer is to:
- get vaccinated against HPV.
- get screened for cervical cancer.
Normally, the Pap test is used to screen for cervical cancer. CancerCare Manitoba's CervixCheck program, in partnership with the Canadian Partnership Against Cancer, is running a pilot project inviting individuals to complete a cervical cancer screening kit in the privacy of their homes.
NOTE: The cervical cancer screening kit is a time-limited project offered to a small number of Manitobans who are due for cervical cancer screening. If you did not receive a letter from CervixCheck about this kit, you are not eligible to receive a kit at this time. To learn more about cervical cancer screening using Pap testing, click here.
If you are a primary care provider, click here to learn more.
Cervical Cancer Screening Kit Instructional Video
To view subtitles, click on the gear icon below and select subtitles. Then select the subtitle language, French or English.
Cervical Cancer Screening Kit Instructions and
Frequently Asked Questions

Frequently Asked Questions
What is CancerCare Manitoba’s CervixCheck program?
CervixCheck is the provincial cervical cancer screening program. We operate a private registry of cervical cancer screening test and follow-up test results for all eligible Manitobans. This is to make sure that anyone who has an abnormal test result gets the follow-up they need. The program also sends letters to invite and remind eligible people to get screened for cervical cancer.
How do you get my information?
Manitoba Health gives CervixCheck the names and addresses of individuals at age 18 or when they become Manitoba citizens. Your information is collected in accordance with regulation of the Public Health Act and the Personal Health Information Act.
Who sees my personal information?
- Your healthcare provider if you provide their contact information.
- The lab that reads your test.
- CervixCheck staff.
Everyone who has access to your information is bound by the Personal Health Information Act (PHIA) and has signed a pledge of confidentiality. For more information about your rights under PHIA contact the Privacy Officer for CancerCare Manitoba at CCMBPrivacyOffice@cancercare.mb.ca or the Manitoba Health Legislative Unit at 204-788-6612.
Will I collect my sample correctly? Will it hurt?
At-home cervix screening is easy and should not hurt. Follow the instructions to take a good sample. Only a small sample from the top of the vagina is needed.
What if I have trouble collecting my sample?
There are a few things you can do to resolve any trouble you have collecting a sample:
- View the instruction video above this section
- Call CervixCheck at 1-855-95-CHECK (1-855-952-4325) during the hours of 8:30am – 4:30pm
- Contact your healthcare provider
How long will it take to get my results and how do I access my results?
You and your healthcare provider will get results about three weeks after you mail in your kit.
What if I get an abnormal result?
An abnormal result does not mean you have or will develop cancer. It does mean a high-risk type of human papillomavirus (hrHPV) has been detected. You will be sent for colposcopy.
What happens if I cannot return my kit the same day I collect my sample?
Make sure to mail your kit no more than 5 days after you collect the sample.
I lost/damaged my kit, can I request a new one?
Yes. To request a new kit you can either:
- Complete an online request on this page, or
- Call CervixCheck at 1-855-95-CHECK (1-855-952-4325).
Will this kit test for anything other than HPV?
No. The kit only tests for high-risk types of HPV. If you require testing for other sexually transmitted infections (STIs), make an appointment with a healthcare provider.
What is the difference between a Pap test and an HPV test?
An HPV test looks for the types of HPV on the cervix that are more likely to become cancer. A Pap test looks for the abnormal cells on the cervix caused by HPV.
You can expect one of the following results from your cervical cancer screening kit:
Normal – A negative result means that high-risk HPV was not detected. You are at low risk for cervical cancer now. You do not need additional testing at this time. Most people will not need a Pap test for three years after a normal HPV test. Contact CervixCheck or your healthcare provider to find out when you should next be screened for cervical cancer.
Abnormal – An abnormal result means that high-risk HPV was detected. This does not mean you have or will get cervical cancer. It means that more treatment is needed to help prevent or treat cervical cancer. CervixCheck will contact you to make an appointment for colposcopy. Be sure to go to the colposcopy appointment.
Invalid - Ann invalid result means that the presence or absence of high-risk HPV could not be determined from the sample. You will be mailed another cervical cancer screening kit to complete.
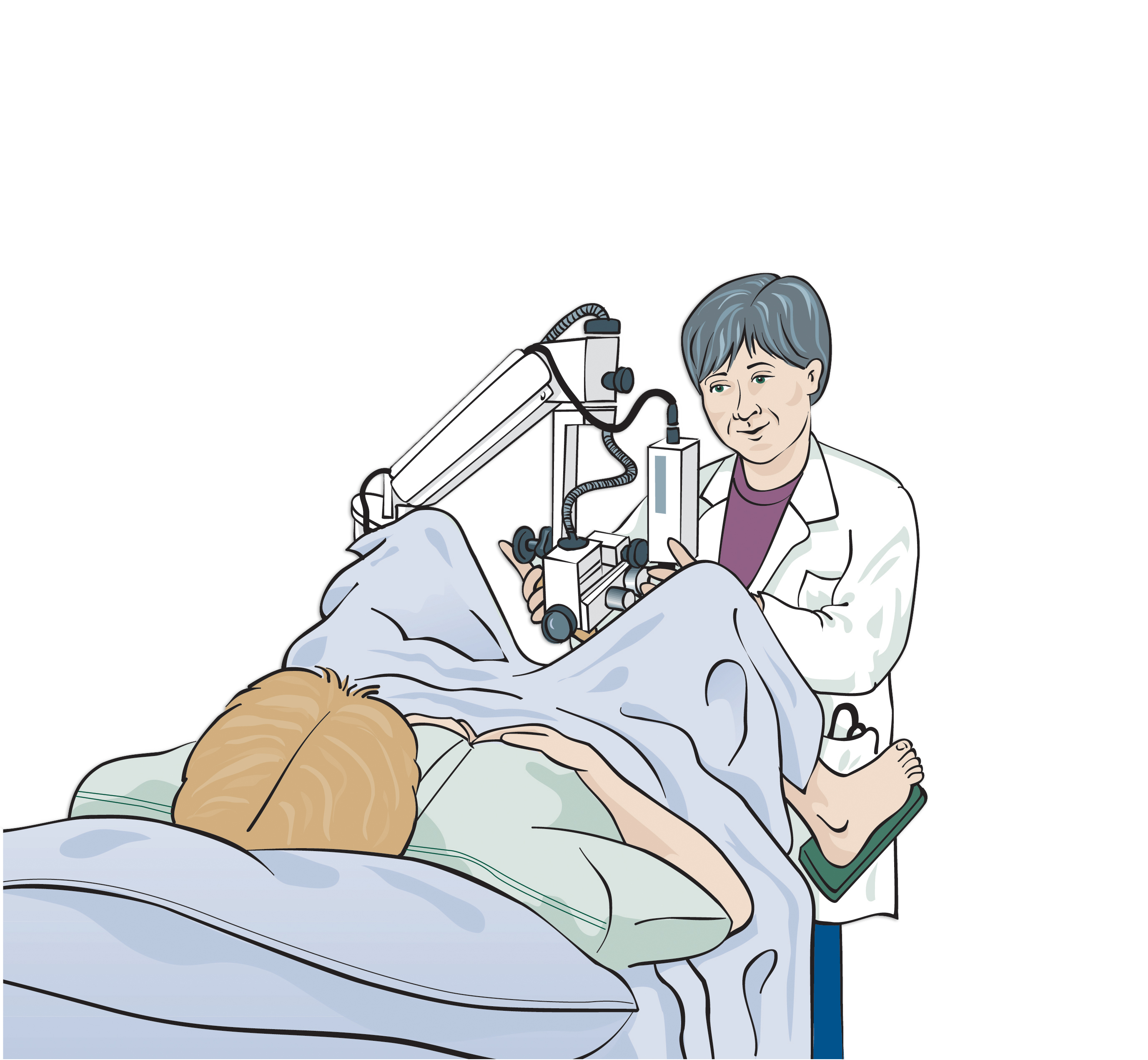
A colposcopy looks at the cervix and vagina using a low-powered magnifying instrument known as a colposcope. The doctor uses a colposcope to look for abnormalities on your cervix to determine if a biopsy or treatment is necessary. If you are pregnant, it is safe to have a colposcopy. The process is similar to a Pap test.
- You will lie down on the exam table and put your feet in supports.
- A speculum will be used to open the vagina so the cervix can be seen.
- Using the colposcope, the doctor magnifies the cervix. The colposcope stays outside the body.
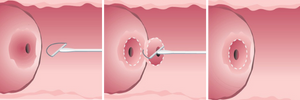
During your colposcopy, the doctor may remove a small tissue sample (biopsy) using an instrument similar to a pair of tweezers. The biopsy is smaller than a quarter of the size of a pencil eraser.
Tell the colposcopy nurse or doctor if you are allergic to iodine.
Will a biopsy hurt?
A biopsy takes less than a minute. Some patients feel nothing. Others describe a pinching feeling or cramps. This usually stops in a few minutes. Your doctor may suggest a pain reliever.
Does a biopsy have any after-effects?
You may have some bleeding (spotting) for a few days. For at least 24 hours after your biopsy, do not put anything into your vagina (e.g. sexual intercourse, tampons, douching).
What types of treatment exist?
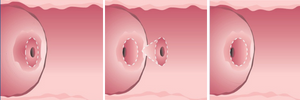
Conization
A conization removes a cone shaped piece of tissue. It is done as a day surgery procedure and requires anesthetic. If cancer cells have been found, it will also determine whether or not these cells have spread to nearby tissues.
LEEP (Loop Electrosurgical Excision Procedure)
After freezing the area with local anesthetic, an electrical wire loop is inserted into the opening of the cervix and the abnormal tissue is removed.
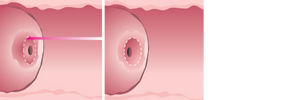
Laser Surgery
Laser surgery uses an intense, narrow beam of light (called a laser beam) to remove abnormal cervical cells. A local anesthetic is used. Watery discharge is a common side effect that may last up to two weeks.
After you are discharged from colposcopy, you should continue with cervical cancer screening (i.e. Pap test) at the recommended interval. Contact CervixCheck or your healthcare provider to find out when you should next be screened for cervical cancer.
What is HPV?
Human papillomavirus (HPV):
- is a common sexually transmitted virus.
- can cause genital warts.
- can cause abnormal cells which can lead to cervical cancer.
- often disappears on its own, only a small number of HPV infections will develop into cancer.
How does HPV spread?
HPV is easily spread through current or past sexual contact, which can include:
- Oral, genital, and/or anal skin-to-skin contact, or
- Sex with shared sex toys.
HPV can pass from person to person regardless of sexual orientation. An HPV infection usually has no signs or symptoms.
Do condoms provide protection against HPV?
Consistent condom use can provide some protection against HPV and other sexually transmitted infections. However, because HPV is easily transmitted via skin-to-skin contact, condoms cannot guarantee complete protection from HPV.
How do I know who gave me HPV?
There is no way to no when you got HPV or who gave it to you. With each new point of sexual contact there is the risk of HPV transmission. Most people who have ever been sexually active will have an HPV infection.
I have been with the same partner for many years, how did I get this?
There is no sure way to know when you got HPV or who gave it to you. Research shows the possibility that HPV can lie dormant and be reactivated in the future. So a person can have HPV for many years before it is detected. Having an HPV infection does not mean that you or your partner have had other partners recently. You or your partner may have had this infection in the distant past; it may have been dormant and only recently reactivated. So even if you are monogamous, the infection may have come back.
What do I tell my partner? Do I need to tell my partner?
Discussing your HPV infection with your partner is an individual decision. It is important to know that HPV transmission is a normal part of being sexually active, and that most sexually active people will have at least one HPV infection at some point in their lives. Having HPV does not mean that you or your partner is having sexual contact outside of your relationship. A person can have HPV for many years before it is detected. Most people have HPV and do not know they have it. HPV is easily transmitted between people through:
- sexual intercourse,
- oral, genital or anal skin-to-skin contact, or
- sex with shared sex toys.
Therefore, it is likely that HPV is being passed back and forth between you and your partner.
If I have HPV, should my partner get tested? Treated?
There is no HPV test available for males. Most HPV infections disappear on their own without any intervention. For women who have sex with women, Pap testing is recommended every 3 years to help prevent cervical cancer caused by HPV. Talk to your partner about whether she is due for a Pap test. CervixCheck can provide women with their Pap test history.
If I am treated in colposcopy, how do I know I won’t catch HPV again?
You don’t. It is possible that any existing infections may reactivate in the future after a period of latency/dormancy. It is also possible that you may be re-infected with new HPV infections if you are exposed. HPV is a normal part of being sexually active. Most HPV infections disappear on their own without any intervention.
Should I get HPV testing every time I have a new partner?
No. Most HPV infections disappear on their own. When HPV persists and grows into cervical cancer, it usually takes 10-20 years. Screening with the Pap test every 3 years allows HPV infections to clear on their own, and at the same time, allows us to detect any abnormal cells on the cervix before they turn into cancer. As well, HPV testing is not routinely available in Manitoba. In other countries that do offer HPV testing, it is recommended every 5 years, even with exposure to new and multiple sexual partners.
HPV testing (HPV triage) is currently offered in Manitoba for female, transgender and non-binary people with a cervix or neo-cervix who are:
- Age 30 and over with an atypical squamous cells of undetermined significance (ASCUS) Pap test result.
- Age 50 and over with a low-grade squamous intraepithelial lesion (LSIL) Pap test result.
Should I get the HPV vaccine now that I know I’m HPV positive?
Patients who have already been exposed to HPV may still benefit from receiving the HPV vaccine, since it is unlikely you have been exposed to all types of HPV in the vaccines. Choosing to get the HPV vaccine is a personal decision. Make an appointment with your health care provider to discuss your suitability for the vaccine.
I’ve had the HPV vaccine, do I still need regular screening?
The HPV vaccine does not protect against all types of HPV that can cause cervical cancer, therefore it is important to continue with screening with Pap tests every 3 years.
To learn more about the HPV vaccine, visit PracticePrevention.ca.
For Primary Care Providers

If you are a primary care provider and would like to learn more about the Cervix Kit project, we invite you to review the Cervical Cancer Screening Kit FAQ for Primary Care Providers.
Contact
For more information contact CervixCheck at:
1-855-95-CHECK (1-855-952-4325)
Interpreter services are available.

